What Causes the White of Your Eyes to Turn Blue
Contents
- Blue sclera
- Blue sclera causes
- Blue sclera symptoms
- Blue sclera diagnosis
- Blue sclera treatment
- Blue sclera prognosis
Blue sclera
Blue sclera is caused by thinness and transparency of the collagen fibers of the sclera that allow visualization of the underlying uvea (Figure 1). The sclera is the white outer coat of the eye, surrounding the iris may be thinned in congenital diseases such as osteogenesis imperfecta 1) . Other diseases associated with blue sclera includes multiple connective tissue disorders, such as brittle cornea syndrome 2) , Marshall and Stickler syndrome 3) , POEMS (polyneuropathy, organomegaly, endocrinopathy, monoclonal protein and skin changes) syndrome 4) , Marfan syndrome, Ehlers–Danlos syndrome, pseudoxanthoma elasticum, and Willems De Vries syndrome, to name a few. Bone and blood disorders also on the list include Diamond–Blackfan anemia, severe iron deficiency anemia, Juvenile Paget's disease, and acid phosphatase deficiency 5) .
Severe forms of osteogenesis imperfecta are most often diagnosed early in life, but mild cases may not be noted until later in life. The blue-gray color of the sclera is due to the underlying choroidal veins which show through. This is due to the sclera being thinner than normal because the defective type I collagen is not forming correctly 6) . The sclera is a dense poorly vascularized connective tissue structure composed of types I, III, IV, V, VI, and VIII collagen, as well as elastin, proteoglycans, and glycoproteins 7) .
In the United States, the incidence of osteogenesis imperfecta is estimated to be one per 20,000 live births. An estimated 20,000-50,000 people are affected by osteogenesis imperfecta in the United States 8) .
People with osteogenesis imperfecta are born with defective connective tissue, or without the ability to make it, usually because of a deficiency of Type I collagen. This deficiency arises from an amino acid substitution of glycine to bulkier amino acids in the collagen triple helix structure. As a result, the body may respond by hydrolyzing the improper collagen structure9) . If the body does not destroy the improper collagen; the relationship between the collagen fibrils and hydroxyapatite crystals to form bone is altered, causing brittleness. As a genetic disorder, osteogenesis imperfecta has historically been viewed as an autosomal dominant disorder of Type I collagen. Most cases have been caused by mutations in the COL1A1 and COL1A2 genes10) . In the past several years, there has been the identification of autosomal recessive forms. At least seven subsets have been described although four major subtypes are most common and range from mild to severe. Individuals with Type I osteogenesis imperfecta have little bone deformity, persistent blue sclera, near normal height by adulthood, and a >50% chance of hearing loss by adulthood. Patients with perinatal lethal (Type II) osteogenesis imperfecta show the greatest severity, with multiple fractures in utero or from the delivery. These patients usually are stillborn or die early. The severity of osteogenesis imperfecta depends on the specific gene defect. Most cases of osteogenesis imperfecta are inherited from a parent. However, some cases are the result of new genetic mutations. A person with osteogenesis imperfecta has a 50% chance of passing on the gene and the disease to his or her children 11) .
Figure 1. Eye anatomy
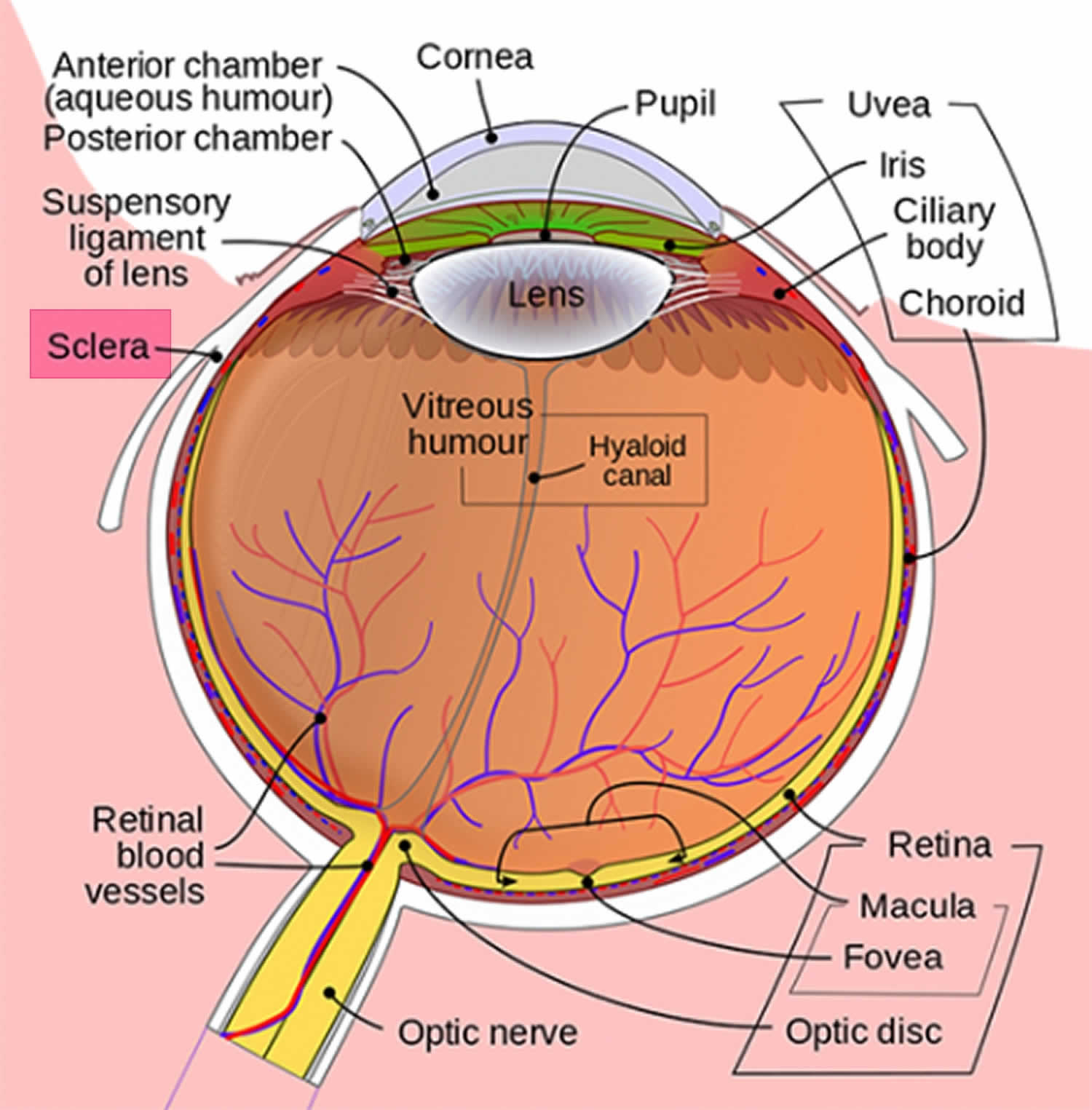
Figure 2. Blue sclera
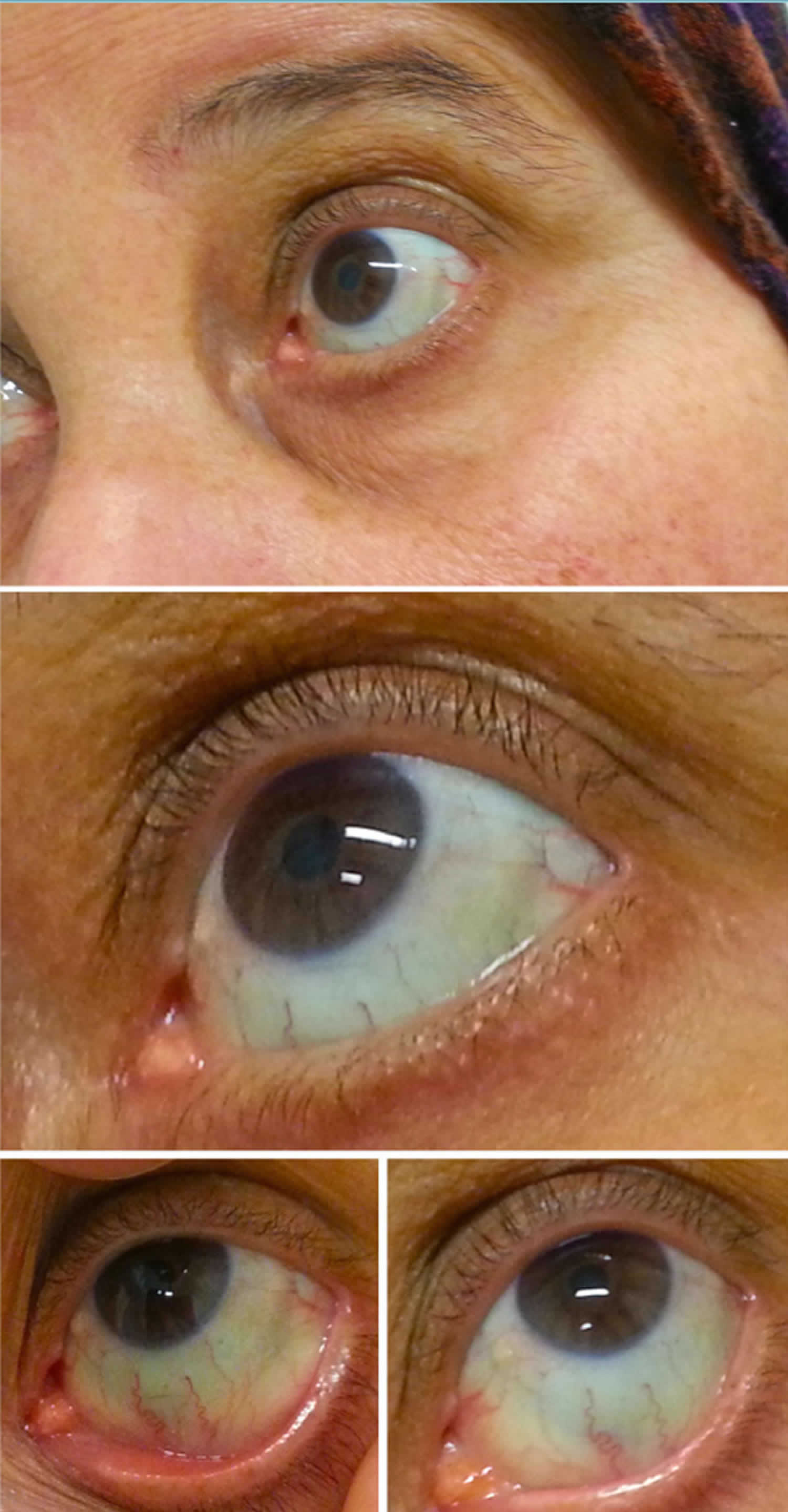
[Source 12) ]
Blue sclera causes
Blue sclera is the most consistent manifestation of osteogenesis imperfecta, which results from a mutation in COLIA1 and COL1A2, coding for type I procollagen. However, classifications of this condition (types IV–VI) have been identified with normal sclerae. Osteogenesis imperfecta is also associated with abnormal fragility of bones and deafness.
Brittle cornea, blue sclera, and red hair are associated with the brittle cornea syndrome, a condition that also presents with skeletal, dental,and skin abnormalities 13) . A missense mutation in ZNF469 has been found to be causative for disease.
Other underlying conditions associated with the formation of blue sclera include Ehlers-Danlos syndrome (type VI), pseudoxanthoma elasticum, cornea plana, peripheral sclerocornea, buphthalmos, keratoconus, keratoglobus, high myopia, ciliary/equatorial staphyloma, oculodermal melanocytosis and microcornea. Rarely, blue sclera occurs with Hallermann-Streiff syndrome, Marfan syndrome, Turner syndrome, Cheney syndrome, Menkes syndrome, pyknodysostosis, brittle corneas, or ectodermal dysplasia.
Blue sclera may also occur in normal infants during the first several months of life; however, persistence of blue discoloration over time may suggest the presence of elevated intraocular pressure. Premature infants frequently demonstrate blue sclerae, particularly those of Caucasian origin.
Blue sclera may also occur in isolation as an inherited autosomal dominant or autosomal recessive anomaly 14) .
Blue sclera symptoms
Blue sclera presents with a bluish appearance to the sclera and may be associated with pathologic or non-pathologic cause. Other ocular characteristics of connective tissue disorders associated with blue sclera include thin cornea, epicanthal fold, myopia, keratoconus, and angioid streaks. Systemic characteristics of connective tissue disorders associated with blue sclera include skin abnormalities, cardiac abnormalities, kyphoscoliosis, joint hypermobility, fragile bones, hearing abnormalities, vascular abnormalities, and gastrointestinal abnormalities 15) .
Blue sclera diagnosis
Diagnostic evaluation of blue sclera involvesexternal examination, slit lamp biomicroscopy,and systemic evaluation for associated disorders.Although no definitive test exists for osteogenesis imperfecta, genetictesting can confirm or exclude known mutations 16) .
Blue sclera treatment
Treatment for blue sclera involves diagnosis and treating the underlying cause. Blue sclera is mostly due to genetic syndromes and to a lesser extent, in nongenetic disorders and may occur as a side effect of medication intake. Blue sclerae are commonly associated with congenital collagen synthesis disorders, such as osteogenesis imperfecta, Marfan syndrome, Ehlers–Danlos syndrome, pseudoxanthoma elasticum, and Willems De Vries syndrome, to name a few. Bone and blood disorders also on the list include Diamond–Blackfan anemia, severe iron deficiency anemia, Juvenile Paget's disease, and acid phosphatase deficiency 17) . Acquired blue sclerae have been described in adults with ocular melanosis, conjunctival melanoma, alkaptonuria and Addison disease. Appropriate referrals to pediatric and orthopedic evaluations may be indicated for non-ocular manifestations 18) .
Genetic counselling for associated inherited disor-ders may be beneficial for patients with blue scleraand other manifestations of systemic disease.
Surgical intervention may be indicated in cases of extreme thinning and perforation. Structural support can be provided by a preserved scleral graft orautologous fascia lata, particularly in cases requiring suturing of a device such as a tube implant 19) . Systemic investigations and treatment should be considered to address underlying pathology.
Blue sclera prognosis
Prognosis varies with the presence of ocular and systemic manifestations of the underlying disorder. Patients with blue sclera are at increased risk for globe rupture or intraoperative scleral perforation during routine eye surgery. Systemic disorders are also prevalent in patients such as carotid-cavernous fistula, arterial rupture, hearing loss,and bone fractures 20) .
References [ + ]
Source: https://healthjade.net/blue-sclera/
0 Response to "What Causes the White of Your Eyes to Turn Blue"
Postar um comentário